Merkel, Eperke Dóra and Schwertner, Walter Richard and Behon, Anett and Kuthi, Luca and Veres, Boglárka and Osztheimer, István and Papp, Roland and Molnár, Levente and Zima, Endre and Gellér, László and Kosztin, Annamária and Merkely, Béla (2023) Predicting the survival benefit of cardiac resynchronization therapy with defibrillator function for non-ischemic heart failure—Role of the Goldenberg risk score. FRONTIERS IN CARDIOVASCULAR MEDICINE, 9. No. 1062094. ISSN 2297-055X
|
Text
fcvm-09-1062094.pdf - Published Version Available under License Creative Commons Attribution. Download (4MB) | Preview |
|
![[img]](https://real.mtak.hu/206186/2.hassmallThumbnailVersion/graphical.abstract.jpg)
|
Text (graphical abstract)
graphical.abstract.jpg - Published Version Available under License Creative Commons Attribution. Download (393kB) | Preview |
Abstract
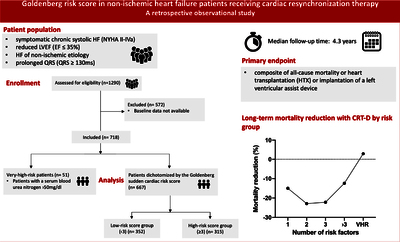
Aims: Primary prevention of sudden cardiac death (SCD) in nonischemic heart failure (HF) patients remains a topic of debate at cardiac resynchronization therapy (CRT) implantation requiring individual risk assessment. Using the Goldenberg SCD risk score, we aimed to predict, which non-ischemic HF patients will benefit from the addition of an implantable cardioverter defibrillator (ICD) to CRT at long-term. Methods: Between 2000 and 2018 non-ischemic HF patients undergoing CRT implantation were collected into our retrospective registry. The Goldenberg risk score (GRS) was calculated by the presence of atrial fibrillation, New York Heat Association (NYHA) class > 2, age > 70 years, blood urea nitrogen > 26 mg/dl and QRS > 120 ms. The primary endpoint was all-cause mortality, heart transplantation or left ventricular assist device implantation. Results: From 667 patients, 347 (52%) underwent cardiac resynchronization therapy-pacemaker (CRT-P), 320 (48%) cardiac resynchronization therapydefibrillator (CRT-D) implantations. During the median follow up time of 4.3 years, 306 (46%) patients reached the primary endpoint (CRT-D 37% vs. CRT-P 63%; p < 0.001). CRT-D patients were younger (64 vs. 69 years; p < 0.001), infrequently females (26 vs. 39%; p < 0.001), and had a lower ejection fraction (27 vs. 29%; p < 0.01) compared to CRT-P patients. After GRS calculation, patients were dichotomized by low (< 3) and high (≥ 3) scores. CRT-D patients with low GRS showed a mortality benefit compared to CRT-P (HR 0.68; 95% CI 0.48–0.96; p = 0.03), high-risk patients did not (HR 0.84; 95% CI 0.62–1.13; p = 0.26). Conclusion: In our non-ischemic cohort, patients with low GRS showed a clear long-term mortality benefit by adding ICD to CRT, however, in high-risk patients no further benefit could be observed
| Item Type: | Article |
|---|---|
| Uncontrolled Keywords: | implantable cardioverter defibrillator, cardiac resynchronization therapy, nonischemic heart failure, risk score, sudden cardiac death |
| Subjects: | R Medicine / orvostudomány > RC Internal medicine / belgyógyászat > RC685 Diseases of the heart, Cardiology / kardiológia |
| Depositing User: | Dr. Annamaria Kosztin |
| Date Deposited: | 07 Oct 2024 12:31 |
| Last Modified: | 07 Oct 2024 12:31 |
| URI: | https://real.mtak.hu/id/eprint/206186 |
Actions (login required)
 |
Edit Item |